Looking down at your phone regularly throughout the day can become a literal pain in the neck. Long periods spent hunched over to reply to email, read a text message or browse the internet may contribute to neck pain, sometimes colloquially referred to as “text” or “tech” neck. This kind of neck pain is reported by more than one in two teenagers and university students, and up to 63% of office workers struggle with neck pain annually.
Prolonged screen time, particularly the way our head and neck are positioned while we engage with our digital devices, is contributing to more than just neck pain. Other clinical features may include headaches, back and shoulder pain, eye strain, dry eyes and other musculoskeletal pains. The effects aren’t solely physical either – “text neck” is also associated with irritability, stress, anxiety and poor communication in school children and adolescents.
Neck pain is very common and, as physiotherapists, we will assess and devise an individualised treatment plan most suitable to your specific presentation. There is evidence to support the use of exercise therapy for some people with neck pain. Today, we look a little deeper into what “text neck” refers to, why it happens, how to spot it and share five examples of exercises that may help manage neck pain.
What Is “Text Neck”?
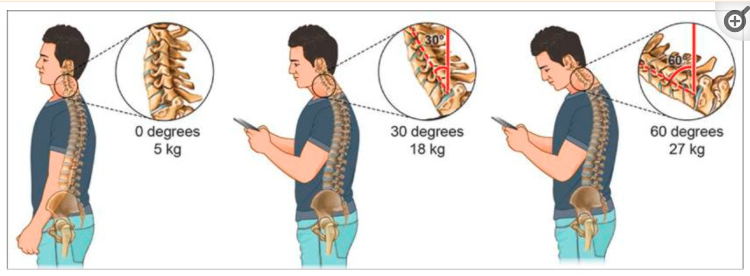
In some people, holding your head forward and downward for extended periods of time can lead to neck pain. “Text neck” refers to pain experienced when you have your neck forwards using devices such as smartphones or tablets.
When your head is upright and looking straight ahead, your neck muscles are only working to support the weight of your head, which is 4.5 – 5.5kgs. At a 15 degree angle, this increases to 12kgs. At a 30 degree angle, your neck muscles must work hard to support over 18kgs. At 45 degrees, the weight that needs to be supported is over 22kgs. Finally, if you’re staring down at 60 degrees, that’s over 27kgs of force on your neck muscles.
What Are The Signs And Symptoms Of “Text Neck”?
The symptoms of “text neck” may include:
- Nagging or sharp pain in the neck or shoulders at the end of the day
- Postural fatigue, or finding it difficult to maintain a healthy posture
- Upper back or neck pain
- General shoulder pain and tightness,
- Constantly holding the head and neck forwards
- Headaches that are made worse when looking down or using the computer.
Exercises To Help
Even though you may not be able to completely eliminate looking down at your phone, there are exercises you can perform that will help relieve some of the tension placed on your neck and back. Generally, we recommend performing the movement sets one to three times a day alongside the support and guidance of a trusted physio who tailors each program to your specific symptoms, circumstances and the results of your comprehensive assessment with us. Here are five examples:
1. Chin Tucks
Chin tucks help to reset the movements that occur when you crane your neck forward towards a screen. Chin tucks can help improve posture and move the head closer to a neutral position, with the ears directly over the shoulders:
- Start by sitting or standing upright while focusing your vision at a specific point across the room.
- Place your index finger on your chin, to help guide your movements.
- Gently move your head back in a purely horizontal fashion so that you tuck your chin backwards against your neck. The motion should create a double chin while you continue to look straight ahead, and not result in your head tilting down to look at your toes.
- Repeat 5-10 times.
2. Neck mobility exercises
To limit the prolonged position of your neck being flexed, it may be helpful to move your neck regularly.
- Sit upright on a chair or stand comfortably with your shoulders relaxed.
- Move your head through a comfortable, pain free range:
- Looking down
- Looking up towards the ceiling bending your neck backwards
- Rotating your head to the right and left
- Tilting your head to the right and left
3. Shoulder Scapular Squeeze
This exercise helps to open up your chest, and activate some of your shoulder blade muscles.
- Sit or stand with your hands clasped behind your head or behind your lower back.
- Open your elbows out to the side and squeeze your shoulder blades back, to feel a stretch in the front of your chest.
- To intensify the stretch, pull your head and shoulders down and backward – continue to look forward, and draw your shoulders away from your ears.
- Hold 10-20 seconds and then slowly release, and repeat three times.
4. Trap Stretches
This exercise helps to relieve tension in the trapezius muscles which span the back of the neck and shoulders, and are responsible for moving and rotating your shoulder blade and extending your neck:
- Look straight ahead, and place your left hand under your thigh, on your chair, to prevent your left shoulder from lifting
- Lift up your right arm and wrap your hand over your head, while tipping your right ear towards your right shoulder. Do not let your left shoulder rise up as you tip your head to the right.
- Hold for 15 to 30 seconds.
- Repeat the exercise on the opposite side, and repeat for 3 times on each side – even if you only have pain on one side.
5. Thoracic Extension
This exercise helps to mobilise the joints of your upper back.
- Sit on a chair with both feet placed on the floor.
- Lift up your arms and place your hands behind your head, with fingers linked together.
- Gently lean forwards in your chair, lowering your stomach towards your thighs, while maintaining a straight back.
- Reach your elbows upwards while tilting your head to look towards the ceiling, while keeping your stomach close to your thighs, curving only your upper back.
- Hold the extension for 5-10 seconds, then slowly release, and repeat 3 times.
Preventing “Text Neck”
Preventing “text neck” starts with the conscious effort to stop leaning the head forward and downward. Limiting your screen time is a great start, but we know this isn’t always possible. When using a digital device:
- Keep it at eye level. You can place some books under your computer screen to bring it closer to eye level, and when you’re using a smartphone, hold it up to your eye height. If you need to be looking down, do so with your eyes, instead of your head.
- Take breaks often. Take 5 minutes every 25 minutes to take a break from the screen, stretch, rest your eyes, and evaluate your posture.
When To See A Physio
If you’re struggling with neck pain from using your computer or smartphone, it may be time to book an appointment with a physiotherapist to help you develop an individualised treatment plan that aims to improve pain and prevent recurrences.
Your physio will carry out a comprehensive assessment, address any underlying conditions, and create a targeted and comprehensive treatment plan to address text neck and protect your overall neck, back and spine health. Having a physio on your team means that they can also support you with targeted manual therapies such as soft tissue massage to enhance your outcomes, answer any questions about your pain to keep you fully supported, and provide you with the best care to enhance your overall neck, back and musculoskeletal health.
To book an appointment with one of our friendly physiotherapists, contact a clinic near you.
References
[1] Prevalence of text neck syndrome and SMS thumb among smartphone users in college-going students
[2] The prevalence of text neck syndrome and its association with smartphone use among medical students in Jeddah, Saudi Arabia
[3] Workplace-Based Interventions for Neck Pain in Office Workers
[4] Text Neck Syndrome in Children and Adolescents